Today, the federal government announced new legislation that lays the groundwork for universal, single-payer pharmacare in Canada and guarantees access in phase one to free birth control and diabetes medications.
This is a victory for reproductive rights in Canada. And long overdue. It’s been 55 years since the birth control pill was legalized in Canada. And since that time, community activists, gender equality organizations and health care providers have worked tirelessly to expand access—inch by inch—to high quality sexual and reproductive health care for all.
With this announcement, the federal government has moved to fill a critical gap in our public health care system and uphold the right of women to choose if and when to have children, through contraception of their choice—regardless of who they are, where they live, their age or disability status, or their income.
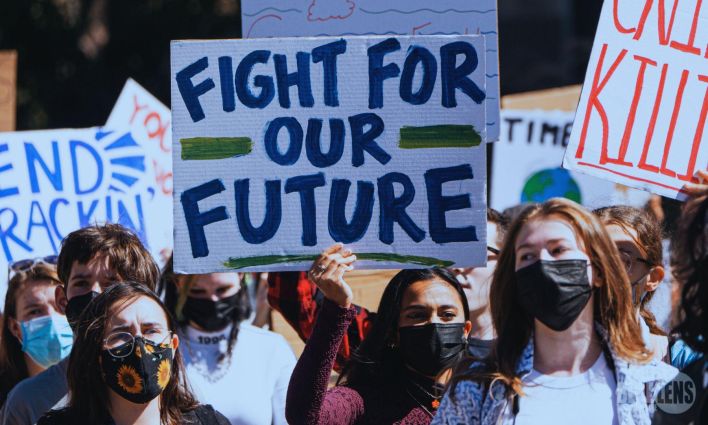
Countries around the world are rolling back reproductive rights and restricting women’s access to essential health care. In the United States, the overturning of Roe v. Wade in 2022 has had vast impacts on abortion access across the US. Reproductive health care and contraception access are in the crosshairs as well, the subject of disinformation campaigns peddled by right-wing media.
Too many Canadians don’t have access to contraception
Access to contraception is fundamental to realizing a wide set of rights relating to sexuality, gender, reproduction, economic security, freedom from violence, and bodily autonomy. This is of critical importance not only to women and those who carry children, but to us all.
Right now, Canada is the only country with universal health care that does not offer coverage for prescription drugs, including contraceptives. Just over half of Canadians have access to an employer-sponsored plan, while 10 per cent purchase private plans of some sort, and another 20 per cent are covered by government-sponsored plans that target specific groups like seniors or households on social assistance.
But one in five people have no drug coverage at all. That’s 7.5 million people—largely low income, from marginalized communities including young people, Indigenous peoples, racialized people, precarious workers, and undocumented migrants and newcomers.
Even among those who have access to a drug plan, many are still not able to afford medications because they can’t afford to pay the upfront deductibles and co-payments. IUDs can cost up to $550 in upfront payment. Oral contraceptive pills are somewhat less expensive—at roughly $240 a year—but that’s still a sizable bill for a student or new immigrant working a gig job.
It’s the same situation for government-sponsored plans that are supposed to support vulnerable groups. A new review of provincial health plans found that contraception coverage varies widely. On average, less than half of provinces provide financial support for birth control for all or most of their populations.
These so-called programs of “last resort” have holes that you can drive trucks through.
Right now, Canada is the only country with universal health care that does not offer coverage for prescription drugs, including contraceptives.
There’s also huge variation in what’s covered with respect to birth control in the other types of plans too. Unlike in the U.S., there are no requirements for government or group plans to cover a range of contraception options such as barrier methods like diaphragms and sponges, hormonal methods like pills and rings, and implanted methods like intrauterine devices (IUDs).
Some plans don’t include birth control at all. Not so long ago this list included Canada Post on the grounds that contraception wasn’t medically necessary. It would be harder to find a more egregious example of sexism than denying coverage to contraception fundamental to women’s quality of life and bodily autonomy—this from a company that spent over 25 years fighting a pay equity dispute with female rural mail carriers.
The high cost of unintended pregnancies
People with insufficient or no contraceptive coverage opt for less expensive and less effective methods because of cost. Young, low-income women, for example, are less likely to use more effective methods of birth control like the pill, and more likely to use no contraception or to rely on condoms alone.
The consequences of unintended pregnancies are profound and lifelong. In Canada, recent studies suggested that upwards of 40 per cent of pregnancies are unintended not only impacting women’s health, future economic security and life choices, but that of their children as well. Some women and their families will have the bandwidth and resources to deal with an unexpected pregnancy. Others will not.
The collective costs are considerable as well. Unintended pregnancies are estimated to cost the Canadian health systems millions of dollars annually. Direct health care costs alone are estimated to be more than $320 million per year. This doesn’t even factor in larger downstream costs to the individuals themselves or to the public purse for supports to families in need.
It’s a wonder why universal contraception has taken so long. There are clear economic benefits. Studies show that for each $1 governments invest in universal contraception, they can save up to $9 in future public expenditures. What’s more, the economic benefits are realized quickly, “with the policy being revenue-neutral by year two and saving money by year three.”
Canadians understand the moral imperative and the economics. There’s huge support for free prescription birth control across the country—across gender, age, parental status, and even political party. Fully 83 per cent agree that free prescription birth control should be available across Canada. Seven out of 10 feel the issue is urgent—especially among young women.
The proposed legislation (Bill C-64) sets out the building blocks for a single-payer universal system including the development of the long-promised national formulary of essential medications and a national bulk purchasing strategy. It commits to long-term, first-dollar coverage for selected prescription drugs and related products—including contraception. The actual details about how people will go about accessing birth control are to be worked out through bilateral agreements with the provinces and the territories.
Even before the legislation dropped, the bluster and dramatics about federal overreach started. Alberta for one has signaled that it won’t participate. “We are not going to allow Ottawa to pick and choose what coverage should be available to Albertans based on issues they find politically palatable,” said Health Minister Adriana LaGrange.
Not a surprise. The Alberta government (and Ontario’s) voted down an opposition motion on no-cost contraception last year, despite public opinion polling showing 74 per cent of Albertans want prescription birth control coverage for all. The government will have to explain to their residents why they aren’t going to take the feds up on their offer.
British Columbians certainly know a good deal when they see it. B.C. was the first to bring in free birth control last spring and since that time, more than 188,000 people have received free contraceptives. Manitoba has just signalled that it’s on board too.
First steps to universal pharmacare?
There are lots of questions still to answer about future access. Which provinces and territories will sign on? What type of delivery models will be funded? How will these programs operate and ensure comprehensive uptake—targeting those most in need? How will the feds measure success? (The government’s track record on monitoring compliance on bilateral agreements is not stellar—ask the child care folks.)
The government has indicated that it doesn’t know how much the program will cost—dependent as this is on what the provinces and territories propose. The commitment to first dollar coverage seems to suggest that the federal government plans to upload the costs of existing public and private insurance plans. But that’s not a given.
And there are certainly other barriers to reproductive health care in Canada—particularly for Indigenous communities, rural residents, people with disabilities, international students and migrant workers, as well as undocumented and homeless people. New Brunswick’s only abortion clinic just shuttered its doors, forced to close because its rent was being doubled and the provincial government’s refusal to extend financial support to community-based service providers.
But we can and should celebrate this victory today. Equitable access to safe, voluntary family planning is a human right, fundamental to ensuring the bodily autonomy of women and advancing gender equality. This is a win for everyone.